Abstract
Introduction: Sickle cell disease (SCD) is the most common inherited blood disorder in the US characterized by vaso-occlusive crisis leading to debilitating pain, organ dysfunction and reduced life expectancy. Despite this, health care staff receive little education on the illness and often feel uncomfortable managing it. The disease is often misunderstood and carries a perceived stigma. Our institution is faced with the additional challenge of lower staff diversity. As part of a larger quality improvement initiative at an institutional level of Sickle Cell Program development, we conducted this project to improve nursing staff level of knowledge and understanding of the disease.
Aims: 1) Identify nursing staff who regularly take care of patients with SCD, evaluate their current knowledge and challenges when caring for patients with SCD, 2) Offer educational modules to address knowledge gaps and implement changes to improve comfort in caring for patients with SCD, 3) Provide a pathway that is reproducible for other institutions.
Methods: The project was conducted at the University of Wisconsin Hospital by a multi-disciplinary SCD team with collaboration from the Nursing Education specialists and the Diversity Equity and Inclusion department. As a pilot cohort, we identified nursing champions who predominantly take care of patients with SCD and offered them to answer an anonymous survey. Based on their responses, educational modules on SCD were designed and video-recorded. Post-surveys were collected for feedback. The Plan-Do-Study-Act methodology was utilized to document progress and conduct tests of change.
QI intervention: Educational module titled "Understanding Sickle Cell Disease and How Nursing Staff Can Help” was designed, video-recorded and uploaded on internal provider platform (U-Learn). Topics included Pathophysiology of SCD, Current treatments, Acute and chronic management of pain, Specialized nursing care for SCD and Addressing disparities, bias and stigma, specifically designed to raise awareness about the new sickle cell team, pain management plans and nursing interventions tailored to our institution. Continuing Education Units (CEU) of 1.5 hours were appointed for their completion. Following the modules, nursing champions answered a post-survey and participated in GRAPES trivia tool, known to improve knowledge and decrease negative attitudes towards patients with SCD. As next step, series of monthly Q&A meetings will be conducted with the nursing champions as an interactive platform for feedback. The nursing champion group will be expanded to form a task force that will serve as SCD patient advocates and help implement ongoing improvements. A best practice alert is being created to facilitate access to patient pain plans in the electronic chart. Patients will be offered surveys to evaluate change in satisfaction with care. Processes implemented at UW will be shared with other regional institutions.
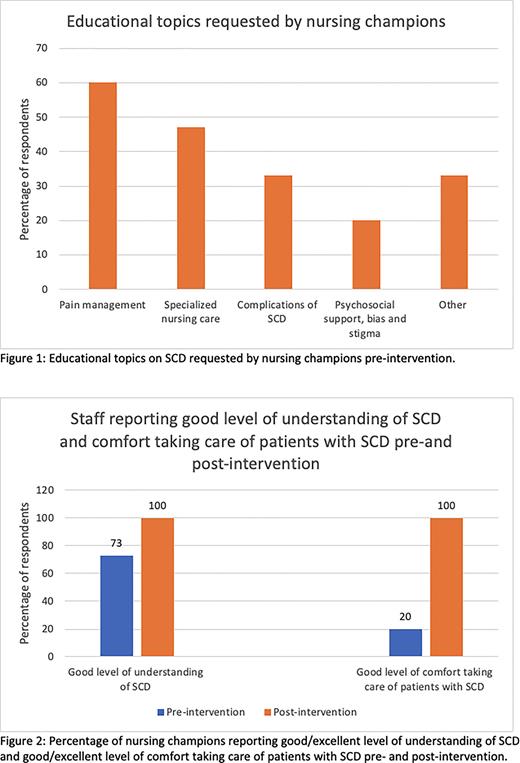
Results: Pre-intervention, 15 (65%) staff members completed the survey. The majority requested education on pain management and nursing care (Fig 1). Preliminary findings show that 20 (87%) nursing champions have signed up and 10 (43%) have completed the modules. 30% of members have completed the post-survey. The proportion of respondents reporting good/excellent disease understanding increased to 100% compared to 73% previously (Fig 2). Proportion of staff who report comfort in taking care of patients with SCD increased from 20% to 100% of the respondents (Figure 2). All respondents felt this module provided them with tools to address systematic racism faced by patients with SCD. Pre-intervention, 80% had acknowledged it's presence.
Conclusion: Our preliminary data from this QI initiative shed light on deficiencies in the care delivered to an underserved patient population at our hospital, and identified areas of improvement. Lack of knowledge and misconceptions lead to low level of comfort by staff leading to sub-optimal care. Creating a nursing champions cohort interested in improving care of patients with SCD, and empowering them to be part of the change, is a feasible strategy to address institutional and systematic challenges. We started with an interactive CEU based, yet flexible educational strategy to engage staff and using their feedback, introduce ongoing improvements. Similar approach can be adopted at other institutions who face similar challenges.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal